Why Should A Medical Oncologist Not Call Himself A Hematologist?
In the ever-evolving field of medicine, specialization plays a crucial role in ensuring that patients receive the highest standard of care. This is particularly true in complex fields like hematology and medical oncology, where the nuances of patient care demand deep, specialized knowledge. Let us see why integration of medical oncology and hematology departments could be problematic and why a medical oncologist should not call themselves a hematologist.
Distinct Areas of Expertise
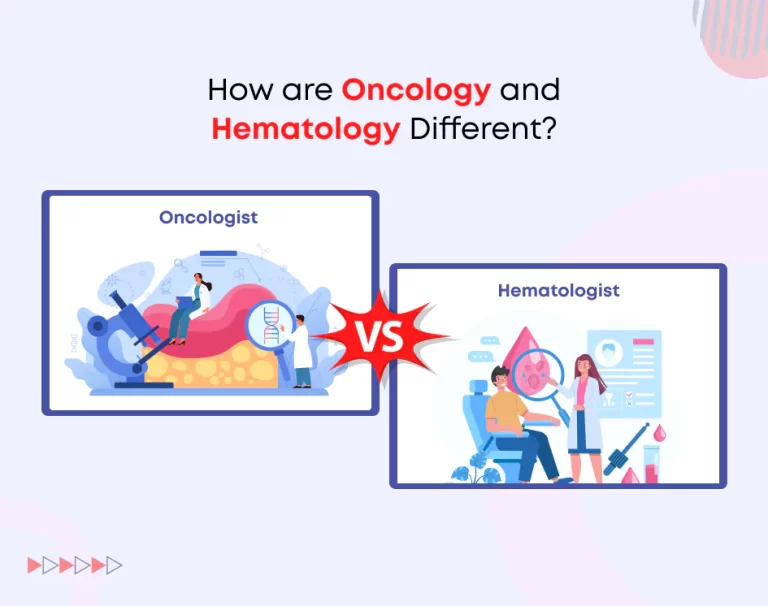
Hematology and medical oncology are two branches of medicine that, while related in their focus on cancer, have fundamentally different areas of expertise.
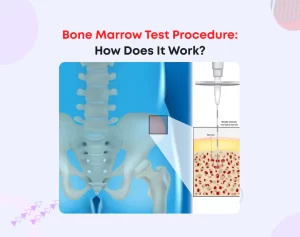
Hematologists in India are specialists in blood disorders, which include a wide range of both malignant (cancerous) and non-malignant conditions. Their expertise lies in diagnosing and treating diseases like leukemia, lymphoma, myelodysplastic syndromes, aplastic anemia, and coagulation disorders. They also manage bone marrow transplants and other complex procedures related to blood and bone marrow. This specialization requires a deep understanding of the hematopoietic system, bone marrow biology, and the specific complications that can arise from blood-related diseases and their treatments.
Medical Oncologists, on the other hand, primarily focus on the management of solid tumors through therapies such as chemotherapy, targeted therapy, and immunotherapy. While they do treat hematologic cancers like leukemia and lymphoma, their expertise is more aligned with the systemic treatment of cancer rather than the broader spectrum of blood disorders. Their training and practice are geared towards managing the progression of cancer, alleviating symptoms, and improving the quality of life for patients with various forms of cancer.
Given these differences, it becomes clear that the scope of practice for each specialty is distinct. A medical oncologist, despite their proficiency in treating cancer, may not have the comprehensive knowledge or experience required to manage the complex, multidisciplinary needs of patients with non-malignant blood disorders or those undergoing bone marrow transplants.
Training and Curriculum Differences
The educational and training paths for hematologists and medical oncologists further highlight the distinction between these two specialties.
Hematologists typically begin their journey with an MBBS (Bachelor of Medicine and Bachelor of Surgery), followed by an MD in Internal Medicine or Pediatrics, depending on whether they want to work primarily with adults or children. After this, they pursue a DM (Doctorate of Medicine) in Clinical Hematology. This advanced training includes a focus on blood disorders, hematopoietic stem cell transplantation, coagulation disorders, hemoglobinopathies (such as Thalassemia and Sickle Cell Disease), and the hematological aspects of systemic diseases. Additionally, hematologists gain extensive experience in lab-based diagnostics, blood banking, and managing complex blood disorders.
Medical Oncologists also start with an MBBS, followed by an MD in Internal Medicine or a related field, and then a DM in Medical Oncology. Their training centers on the diagnosis and treatment of cancer, particularly solid tumors, with an emphasis on chemotherapy, targeted therapy, immunotherapy, and palliative care. While they do treat hematologic malignancies, their exposure to non-malignant blood disorders is limited.
These distinct training paths underscore the specialized knowledge that each group of professionals brings to their practice.
A medical oncologist may be highly skilled in managing cancer treatment, but they do not possess the same depth of expertise in hematology as someone who has undergone the rigorous training required to become a hematologist.
Regulatory and Ethical Considerations
According to Indian medical guidelines, a physician’s specialization is determined by their completed training and certified qualifications.
For a medical oncologist, this means that while they are qualified to manage cancer, they are not certified or trained to handle the broader spectrum of hematology, especially non-malignant blood disorders. Thus, it would be both legally and ethically inappropriate for a medical oncologist to present themselves as a hematologist. Doing so could mislead patients, compromise the quality of care, and expose the practitioner and the institution to legal liabilities.
Ethically, physicians are required to accurately represent their qualifications to avoid misleading patients. Patients seeking care from a hematologist expect to receive specialized care from someone with the requisite training and expertise in blood disorders. If a medical oncologist were to assume this role without the proper qualifications, it could lead to suboptimal patient outcomes and potential malpractice claims.
Potential Risks to Patient Care
The integration of medical oncologists into a hematology department, or the blurring of lines between these two specialties, can have serious implications for patient care. Hematology patients often present with complex and life-threatening conditions that require a precise and nuanced approach. The management of these conditions often involves rigorous diagnostic and therapeutic procedures that demand a coordinated effort led by a hematologist.
For example, managing graft-versus-host disease (GVHD) in bone marrow transplant patients requires a deep understanding of hematology and transplant immunology. A medical oncologist, whose expertise is centered on solid tumors, may not have the necessary experience to handle such complex scenarios. This lack of expertise could lead to fragmented care, increased risk of complications, and ultimately poorer patient outcomes.
Legal and Reputational Risks
Allowing medical oncologists to present themselves as hematologists could also expose institutions to significant legal and reputational risks. Indian medical regulations clearly stipulate that specialists must operate within their certified areas of expertise. Violating these guidelines by misclassifying a medical oncologist as a hematologist could result in legal repercussions.
In today’s information age, even the perception of false representation can lead to loss of trust among patients, referring physicians, and the broader medical community.
Conclusion
Hematology and medical oncology are distinct specialties, each with its own specific focus, training, and scope of practice. While there is some overlap in the treatment of hematologic malignancies, the comprehensive care of blood disorders and bone marrow transplants requires the expertise of a trained hematologist.
For these reasons, a medical oncologist should not and cannot ethically or legally call themselves a hematologist. To ensure the highest standard of patient care and to maintain trust in the medical profession, it is crucial that practitioners accurately represent their qualifications and operate within the boundaries of their certified specialties.