When Is Platelet Transfusion Needed?
Platelet transfusion is a critical medical intervention used to treat various conditions that affect blood clotting. But when exactly is platelet transfusion needed, and what does it include? In this comprehensive guide, we’ll delve into the topic of platelet transfusion and explore the circumstances that warrant it. We will also talk about the reasons behind its necessity. Are you a patient, caregiver, or simply curious about this medical procedure? Join us as we get to know what platelet transfusion is and shed light on its significance.
What Are Platelets and Their Role in Blood Clotting?
Platelets, also known as thrombocytes, are small cell fragments present in the blood. They play a crucial role in the process of blood clotting, or hemostasis. When a blood vessel is damaged, platelets rush to the site of injury and form a plug to stop bleeding. Additionally, they release various substances. The released ones promote clot formation and help stabilize the clot until the vessel heals.
Key Functions of Platelets
Below are the essential functions of platelets:
Formation of Blood Clots
Platelets adhere to the site of injury. Further, they aggregate together to form a temporary seal, preventing further blood loss.
Release of Clotting Factors
Platelets release chemicals that facilitate the coagulation process, promoting the formation of a stable clot.
Stabilization of Clots
Platelets help strengthen and stabilize the clot, preventing premature dissolution and ensuring effective wound healing.
The role of platelets lays the foundation for comprehending the necessity of platelet transfusion in certain medical scenarios.
When Is Platelet Transfusion Needed?
Platelet transfusion may be necessary in the following situations:
Treatment of Thrombocytopenia
A condition characterized by a low platelet count in the blood refers to Thrombocytopenia. This can occur due to various reasons, including chemotherapy, radiation therapy, bone marrow disorders, and certain medications. Platelet transfusion may also be required to prevent or control bleeding in cases of severe Thrombocytopenia. Why? As the platelet count drops to dangerously low levels in these cases.
Management of Platelet Dysfunction
Platelet dysfunction occurs when platelets are unable to function properly, even when their count is normal. This can occur in conditions such as von Willebrand disease, hemophilia, and other inherited or acquired platelet disorders. Platelet transfusion may be necessary to provide functional platelets and support normal blood clotting in these cases.
Surgical Procedures
Certain surgical procedures may necessitate platelet transfusion to support hemostasis and prevent excessive bleeding. It may be particularly for those surgical processes involving major blood loss or extensive tissue damage. This is especially true for surgeries involving the liver, spleen, or cardiovascular system. Because the risk of bleeding complications is higher in these cases.
Treatment of Acute Bleeding
Platelet transfusion may be used as part of the emergency management protocol. It is done to control bleeding and stabilize the patient’s condition. This is utilized in cases of acute bleeding or hemorrhage. For example, trauma-related injuries or gastrointestinal bleeding.
Management of Platelet Function Disorders
Platelet function disorders, such as aspirin or clopidogrel resistance, may require platelet transfusion. As a result, it can overcome the impaired response to antiplatelet medications. Likewise, it restores normal clotting function.
Platelet transfusion plays a crucial role in managing various conditions, ensuring better patient outcomes and recovery.
Factors Considered Before Platelet Transfusion
Before administering a platelet transfusion, healthcare providers consider various factors, including:
Platelet Count
The patient’s platelet count helps determine the need for transfusion and the appropriate dosage.
Bleeding Risk
The severity and location of bleeding, as well as the underlying cause, influence the decision to transfuse platelets.
Patient’s Clinical Condition
The patient’s overall health status, medical history, and response to previous transfusions are taken into account.
Underlying Disorders
Any underlying medical conditions or medications that may affect platelet function or increase bleeding risk are considered.
These factors ensure that platelet transfusion is administered safely and effectively.
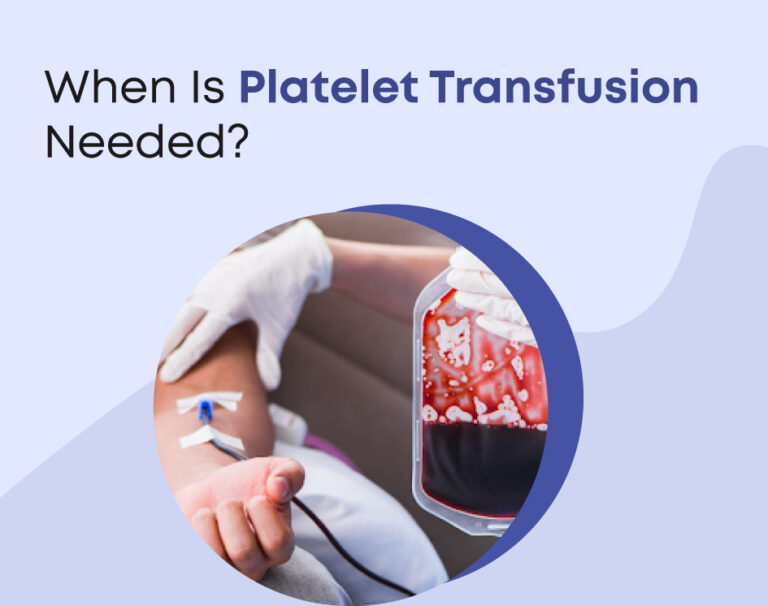
Platelet Transfusion Procedure
The platelet transfusion process typically involves the following steps:
Blood Compatibility Testing
Prior to transfusion, the recipient’s blood type is determined. Along with that, compatibility testing is performed to ensure a safe transfusion.
Platelet Collection
Platelets may be obtained from donated whole blood or through a process called apheresis. Here, specific blood components, including platelets, are collected from a donor and transfused to the recipient.
Transfusion Administration
Platelets are transfused intravenously (IV) into the recipient’s bloodstream over a period of time. They usually range from 30 minutes to a few hours, depending on the dosage and the patient’s condition.
Monitoring
Throughout the transfusion process, the patient’s vital signs and clinical status are closely monitored. This is done in order to check for any signs of adverse reactions or complications.
The above protocols during platelet transfusion are essential for promoting patient safety and optimal outcomes.
Risks and Complications of Platelet Transfusion
While platelet transfusion is generally considered safe, there are potential risks and complications, including:
- Allergic Reactions
A few people might encounter allergic reactions to the platelets they receive during transfusion. It ranges from mild itching or rash to more severe symptoms such as difficulty breathing or anaphylaxis.
- Transfusion-related Acute Lung Injury (TRALI)
TRALI is a rare but serious complication. It is characterized by sudden respiratory distress and lung injury following transfusion.
- Transmission of Infections
Stringent screening measures are in place to minimize the risk. Yet, there is a slight possibility of transmitting infections through transfused platelets.
- Febrile Non-hemolytic Reactions
Some patients may develop fever and chills due to immune-mediated reactions to the transfused platelets.
It’s crucial to be aware of the risks and complications of platelet transfusion for a safe healthcare journey.
Winding Up
Platelet transfusion is a vital therapeutic intervention. It is used to manage various conditions associated with impaired blood clotting. If you have any questions or concerns about platelet transfusion, be sure to discuss them with your healthcare provider or contact us for personalized guidance and support.