Monkeypox (Mpox): Causes, Symptoms, Diagnosis & Treatment
In recent years, public health experts have raised the alarm over the rise in monkeypox cases, an infectious disease that, while less severe than smallpox, can lead to serious health complications. As the world becomes increasingly aware of emerging diseases, it is essential to understand the causes, symptoms, diagnosis, and treatment of monkeypox. Let’s see how to manage and prevent this viral infection.
What is Monkeypox?
Monkeypox is a zoonotic virus, which means it is transmitted from animals to humans. It belongs to the Orthopoxvirus genus, which also includes smallpox (variola virus) and cowpox. First discovered in 1958 among laboratory monkeys, the disease’s name is somewhat misleading, as monkeys are not the primary animal reservoir. Rodents, such as squirrels and rats, are thought to be the primary carriers of the virus.
There are two distinct strains of the monkeypox virus: the West African strain and the Congo Basin strain. The West African strain has a lower mortality rate, with about 1 in 10 people infected dying, while the Congo Basin strain is more virulent, with a fatality rate closer to 1 in 100. These two strains behave differently in terms of transmission and severity, making it important to distinguish which strain is responsible during an outbreak.
Causes of Monkeypox
Monkeypox is caused by the monkeypox virus, and its transmission primarily occurs through close contact with infected animals or humans. The virus can spread via respiratory droplets, bodily fluids, or contact with contaminated materials, such as bedding or clothing used by an infected person. While monkeypox is not as easily transmissible as diseases like COVID-19, it still poses a significant risk of human-to-human transmission, particularly in close, crowded settings.
Animal-to-human transmission often occurs through direct contact with the blood, bodily fluids, or lesions of infected animals. Handling animals, particularly wild rodents or primates, can lead to exposure, making zoonotic spillover events possible in regions where the virus circulates in animal populations.
Symptoms of Monkeypox
Monkeypox symptoms generally appear between 5 and 21 days after exposure to the virus, with the initial stage closely resembling flu-like symptoms. Patients often experience:
Fever: The sudden onset of fever is one of the first signs of infection.
Muscle aches and headaches: These symptoms are common and are typically accompanied by general fatigue.
Swollen lymph nodes: A key distinguishing feature of monkeypox, as swollen lymph nodes are rarely seen in other poxvirus infections such as smallpox.
Chills and exhaustion: These symptoms may appear before or in conjunction with the rash.
Within 1 to 3 days of the fever, a distinctive rash develops, beginning on the face and then spreading to other parts of the body, including the palms of the hands and soles of the feet. The rash progresses through different stages: from macules (flat lesions) to papules (raised lesions), vesicles (fluid-filled lesions), and pustules (pus-filled lesions). After several days, the lesions crust over and eventually fall off.
The rash is perhaps the most telling sign of monkeypox, and its pattern of development closely resembles that of smallpox. However, unlike smallpox, monkeypox infections usually result in milder cases and have a lower fatality rate.
How is Monkeypox Diagnosed?
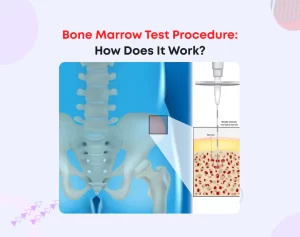
Given the similarity of monkeypox to other poxviruses, a definitive diagnosis requires laboratory testing. Health professionals typically take samples from the skin lesions, including the fluid from vesicles or pustules, or crusted scabs, which are then tested using Polymerase Chain Reaction (PCR) technology. PCR testing is preferred due to its high sensitivity and specificity.
In some cases, a blood test may be necessary to differentiate monkeypox from other infections, especially when the rash has not yet appeared. It is crucial to perform a thorough clinical examination and review the patient’s medical history, including recent travel to regions where monkeypox is known to circulate or contact with individuals diagnosed with the virus.
Biopsy of the skin lesions may also be considered in certain cases, particularly when the diagnosis is uncertain or other conditions, such as chickenpox or measles, need to be ruled out. Early detection through accurate diagnostics is key to preventing further transmission and providing appropriate treatment.
Treatment of Monkeypox
Although monkeypox is typically a self-limiting disease, meaning it resolves on its own within 2 to 4 weeks, severe cases can occur, particularly in individuals with weakened immune systems or underlying health conditions. The goal of treatment is to manage symptoms, prevent complications, and reduce the risk of long-term consequences, such as scarring or secondary infections.
Patients are encouraged to rest, stay hydrated, and eat a nutritious diet to maintain overall health during the recovery period. Supportive care, such as managing fever and pain with over-the-counter medications, may be helpful. In more severe cases, antiviral treatments may be necessary.
How to Prevent Monkeypox?
Prevention strategies for monkeypox focus on reducing exposure to the virus. This involves avoiding contact with animals that may harbor the virus, especially in regions where monkeypox is endemic. Public health campaigns play a crucial role in educating communities about the risks of handling wild animals, particularly rodents and primates, and promoting practices such as wearing protective gear when handling animals.
For healthcare workers and those in close contact with infected individuals, infection control measures are vital. These include wearing personal protective equipment (PPE), practicing good hand hygiene, and properly disinfecting contaminated surfaces and materials.
Vaccination
In the event of an outbreak, vaccination may be recommended for those at risk. In some regions, the smallpox vaccine is offered as a preventive measure, as it has demonstrated effectiveness in providing cross-protection against monkeypox. Post-exposure vaccination, ideally administered within four days of exposure, can help reduce the severity of the disease or prevent it altogether.
The Intersection of Monkeypox and Hematology
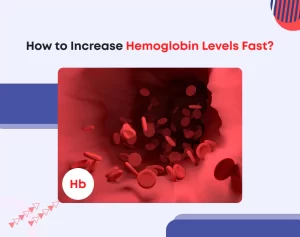
The connection between monkeypox and hematology lies in the virus’s impact on the blood and immune system. One of the hallmark symptoms of monkeypox is swollen lymph nodes, which are part of the lymphatic system—a crucial component of the immune system that helps fight infections.
Hematologists, who specialize in blood and lymphatic diseases, may be involved in the management of monkeypox cases, particularly in patients who develop complications affecting the blood, such as thrombocytopenia (low platelet count) or anemia.
Furthermore, the study of monkeypox and other viral infections contributes to a broader understanding of how viruses interact with the immune system and the blood. This knowledge is invaluable in developing treatments and preventive strategies for various infectious diseases.
Conclusion
Monkeypox is a zoonotic disease with serious public health implications, particularly as global travel and wildlife-human interactions increase. While monkeypox is generally milder than smallpox, it is important to remain vigilant, especially with the potential for severe cases and complications. By understanding its causes, symptoms, diagnosis, and treatment, we can better prepare for and respond to future outbreaks.
Early diagnosis, supportive care, and targeted antiviral treatments can mitigate the disease’s impact, while preventive measures, such as vaccination and education, will be key to controlling its spread. As we continue to face the threat of emerging infectious diseases, a proactive approach to managing monkeypox will help protect public health on a global scale.