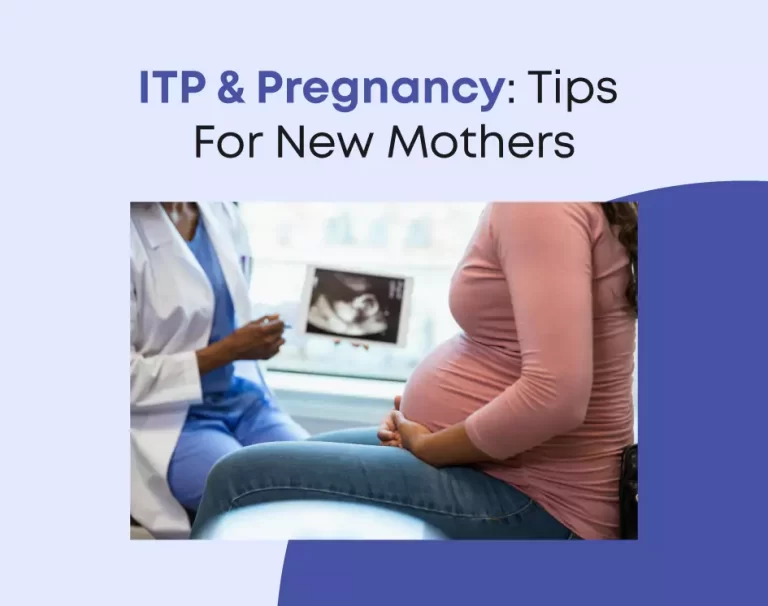
ITP & Pregnancy: Tips For New Mothers
Pregnancy is a beautiful and transformative experience, but it can also present unique challenges, especially for mothers with immune thrombocytopenia (ITP). In this guide, we’ll explore everything you need to know about managing ITP during pregnancy and beyond. From understanding the condition to practical tips for a healthy pregnancy, we’ve got you covered. So, dive in and empower you with the knowledge and resources to navigate ITP and pregnancy with confidence.
Understanding ITP and Its Impact on Pregnancy
Immune thrombocytopenia (ITP) is a rare autoimmune disorder characterized by low platelet levels in the blood. During pregnancy, the body undergoes significant changes. This includes alterations in the immune system, which can exacerbate ITP symptoms. The key points you should be aware of are as follows:
- Impact of Pregnancy on ITP
Pregnancy can either improve or worsen ITP symptoms. It’s essential to monitor platelet levels regularly and work closely with your healthcare provider to manage the condition effectively.
- Risks and Complications
Mothers with ITP may face increased risks of bleeding complications during pregnancy, childbirth, and postpartum. Understanding these risks and taking proactive measures is crucial for a safe pregnancy journey.
- Consulting with Healthcare Providers
Before conception, discuss your pregnancy plans with your hematologist and obstetrician. They can provide personalized guidance and recommend appropriate treatment options to optimize your health and minimize risks.
- Managing ITP During Pregnancy
Implementing strategies to manage ITP during pregnancy is essential for ensuring a healthy outcome for both mother and baby. Do call us to speak to our expert hematologist and get recommend medications, lifestyle modifications, and monitoring protocols tailored to your individual needs.
Knowing about the impact of ITP on pregnancy is vital for expectant mothers. It guides them to navigate this journey with informed decisions and proactive management.
Tips for Managing ITP During Pregnancy
Navigating pregnancy with ITP requires careful planning and proactive management. Here are some practical tips to help you stay healthy and minimize complications:
- Regular Monitoring
Attend scheduled prenatal appointments and follow-up visits with your hematologist to monitor platelet levels closely. Regular monitoring allows for early detection of any changes and timely intervention if needed.
- Medication Management
Work with your doctor to develop a tailored treatment plan that balances the need for managing ITP with the safety of your baby. Some medications used to treat ITP may be safe during pregnancy. Meanwhile, others may need adjustments or alternatives.
- Healthy Lifestyle Choices
Stick to a balanced diet packed with nutrients crucial for you and your baby’s well-being. Incorporate foods high in iron and folate to support healthy blood cell production. Additionally, engage in gentle exercises approved by your healthcare provider to stay active and relieve stress.
- Avoiding Triggers
Identify and avoid activities or situations that may increase the risk of bleeding or exacerbate ITP symptoms. This may include avoiding contact sports, strenuous activities, and certain medications that can affect platelet function.
- Seeking Emotional Support
Pregnancy can be an emotional rollercoaster, especially when managing a chronic condition like ITP. Feel free to reach out to mental health professionals, support groups, or trusted loved ones for assistance and support. They will help you cope with stress and anxiety.
Successfully managing ITP during pregnancy is achievable with regular monitoring. Medication management, healthy lifestyle choices, and seeking emotional support are also necessary for a smoother journey ahead.
Preparing for Labor and Delivery
As your due date approaches, it’s essential to discuss your birth plan and labor preferences with your doctor. Below are some important factors for mothers dealing with ITP:
- Birth Plan Discussion
Have an open and honest conversation with your obstetrician about your ITP diagnosis and any specific concerns you may have regarding labor and delivery. Discuss pain management options, delivery methods, and potential interventions.
- Platelet Counts
Monitor platelet levels closely in the weeks leading up to your due date. Your healthcare provider may recommend additional blood tests or interventions. For example, intravenous immunoglobulin (IVIG) infusions or corticosteroid therapy. These tests will assist in boosting platelet counts if necessary.
- Hospital Birth
Consider giving birth in a hospital setting equipped to handle potential complications associated with ITP, like excessive bleeding. Ensure that your healthcare team is aware of your ITP diagnosis. Besides, they should have a plan in place for managing any emergencies.
- Labor Support
Surround yourself with a supportive birth team, including healthcare providers, partners, and labor coaches. Choose those who understand your medical history and are prepared to advocate for your needs during labor and delivery.
As you prepare for labor and delivery, open communication with your healthcare team and careful monitoring of platelet levels are crucial for a safe and successful birth experience with ITP.
Postpartum Care and Recovery
The postpartum period is a critical time for mothers with ITP. Why? As it carries an increased risk of bleeding complications. Below are ways to prioritize your well-being and health during this phase:
- Close Monitoring
Keep monitoring your platelet levels during the weeks after giving birth, as they can fluctuate during the postpartum period. Attend follow-up appointments with your healthcare provider to ensure that your recovery is progressing smoothly.
- Rest and Recovery
Give yourself plenty of time to rest and recover following childbirth. Steer clear of demanding tasks and focus on self-care activities like light exercise, nourishing meals, and sufficient sleep.
- Breastfeeding Considerations
Consult with your healthcare provider about the safety of breastfeeding while managing ITP. Some medications used to treat ITP may pass into breast milk. So, discuss the potential risks and benefits to make an informed decision.
- Emotional Well-being
The postpartum period can be emotionally challenging, so prioritize your mental health and seek support if needed. Reach out to your healthcare provider, counselor, or support groups for assistance with coping strategies and emotional support.
In the postpartum phase, continued monitoring of platelet levels, prioritizing rest and recovery, discussing breastfeeding considerations, and addressing emotional well-being are essential for mothers with ITP. Doing all these will help to navigate this critical period safely and effectively.
Summing Up
Navigating pregnancy with ITP presents unique challenges. Yet, by engaging in thorough planning and proactive management, one can experience a wholesome and gratifying pregnancy voyage. By understanding the impact of ITP on pregnancy, implementing practical tips for managing the condition, and collaborating closely with your healthcare team, you can optimize your health and well-being for both you and your baby. Remember, you’re not alone in this journey—seek support from loved ones and healthcare professionals, and trust in your strength as a new mother facing ITP with resilience and determination.