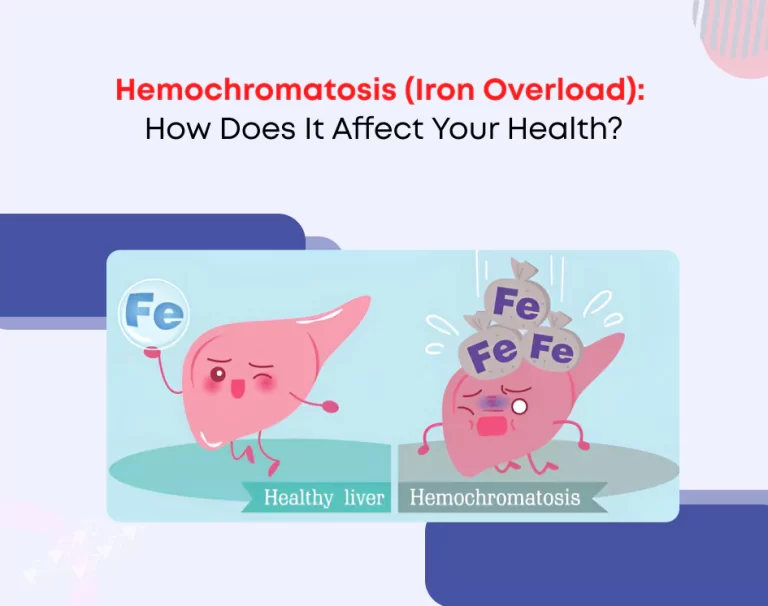
Hemochromatosis (Iron Overload): How Does It Affect Your Health?
Iron is vital for the body, as it helps carry oxygen in the blood and supports the production of healthy red blood cells. But did you know that having too much iron in your blood can be harmful? This is the case with a condition called hemochromatosis, where the body absorbs too much iron, leading to potential damage to organs like the liver, heart, and pancreas.
While it might sound complicated, understanding hemochromatosis doesn’t have to be. In this post, we’ll break down what hemochromatosis is, how it happens, what to look out for, and how it can be treated.
What is Hemochromatosis?
Hemochromatosis is a condition in which the body absorbs more iron than it needs. This extra iron is stored in different organs, mainly the liver, heart, and pancreas. Over time, this buildup of iron can damage these organs and lead to serious health problems.
The condition can be caused by a genetic mutation (meaning it’s inherited from your parents) or by other factors like blood disorders or excess iron in the diet (though this is less common).
Causes of Hemochromatosis
There are two main types of hemochromatosis:
Primary hemochromatosis is the most common type. It is caused by a genetic mutation that causes the body to absorb too much iron from the food it eats. It’s inherited, meaning if your parents carry the gene for it, you might have it, too.
Secondary Hemochromatosis happens due to other conditions, like chronic anemia (a blood disorder) or repeated blood transfusions. It can also be caused by taking too many iron supplements, though this is rare.
The primary form, which is caused by a genetic mutation, is what most people mean when they talk about hemochromatosis.
Symptoms of Hemochromatosis
The tricky thing about hemochromatosis is that the symptoms can be slow to appear and pretty general. This means it can be hard to tell if you have it just from the symptoms alone.
Common signs of iron overload include:
Fatigue: Experiencing persistent tiredness or lack of energy despite having sufficient rest or sleep.
Joint pain: Discomfort in the joints, often in the knuckles, hips, or knees.
Abdominal discomfort: You might feel pain or a sense of fullness in your stomach, especially in the area where your liver is (on the right side, just under your ribcage).
Changes in skin color: Some people with hemochromatosis develop a bronze or grayish tint to their skin.
Liver problems: Over time, excess iron can damage your liver, leading to cirrhosis (scarring) or even liver failure.
Diabetes: Excess iron can damage the pancreas, which affects insulin production and can lead to diabetes.
Heart problems: Iron can build up in the heart, causing irregular heartbeats (arrhythmias) or even heart failure.
If you’re experiencing any of these symptoms, it doesn’t necessarily mean you have hemochromatosis, but it’s a good idea to talk to your doctor for further tests.
How Is Hemochromatosis Diagnosed?
If your doctor suspects you might have hemochromatosis, they’ll start by checking your iron levels through a blood test. The two main tests to look at are:
Serum ferritin: This measures the amount of iron stored in your body.
Transferrin saturation: This shows how much iron is in your blood compared to how much is available for your body to use.
If these levels are high, it could be a sign that you have too much iron in the blood. However, these tests alone don’t confirm hemochromatosis, so the next step is often genetic testing to see if you have mutations in the gene that causes the condition.
In some cases, doctors may also perform imaging tests or even a liver biopsy to determine how much iron has built up in the liver and whether it has caused damage.
Treatment
The good news is that hemochromatosis can be managed effectively if caught early. The main goal of treatment is to reduce the iron levels in your body to prevent damage to your organs.
The most common treatment is phlebotomy, which is the process of regularly donating blood. Each time you donate blood, you remove some iron along with it. Initially, you may need to have this done once or twice a week, but as your iron levels decrease, it will be done less frequently—maybe once a month or even less often.
If phlebotomy isn’t an option or isn’t enough, doctors may recommend iron chelation therapy. This involves taking medication that binds to the excess iron and helps your body remove it.
Along with medical treatment, you may also be advised to make lifestyle changes:
Avoid iron supplements: People with hemochromatosis should not take iron supplements unless prescribed by a doctor, as this can worsen the condition.
Limit vitamin C: Vitamin C helps the body absorb iron, so you should limit vitamin C supplements or avoid consuming large amounts of vitamin C-rich foods (like citrus fruits) when eating iron-rich meals.
Limit alcohol: Since alcohol can cause liver damage and people with hemochromatosis are already at risk for liver problems, cutting back on alcohol is usually recommended.
Living with Hemochromatosis
While hemochromatosis can lead to serious health issues if not treated, it’s possible to live a normal life with the condition. Early detection is crucial for preventing organ damage. Once iron levels are managed through phlebotomy or other treatments, people with hemochromatosis can lead a healthy, active life.
If you have hemochromatosis, it’s important to stay on top of your health by:
- Regular blood tests help monitor your iron levels.
- Following your doctor’s advice on diet and treatment.
- Avoiding alcohol and iron-rich supplements unless told otherwise.
Conclusion
Hemochromatosis is a serious condition, but it’s manageable with early detection and treatment. If you have a family history of the disease or experience symptoms like unexplained fatigue, joint pain, or skin changes, it’s important to talk to your doctor. With the right treatment, most people with hemochromatosis can live healthy, full lives.
If you think you might be at risk, don’t hesitate to get tested; call us—it could make a big difference to your health in the long run.