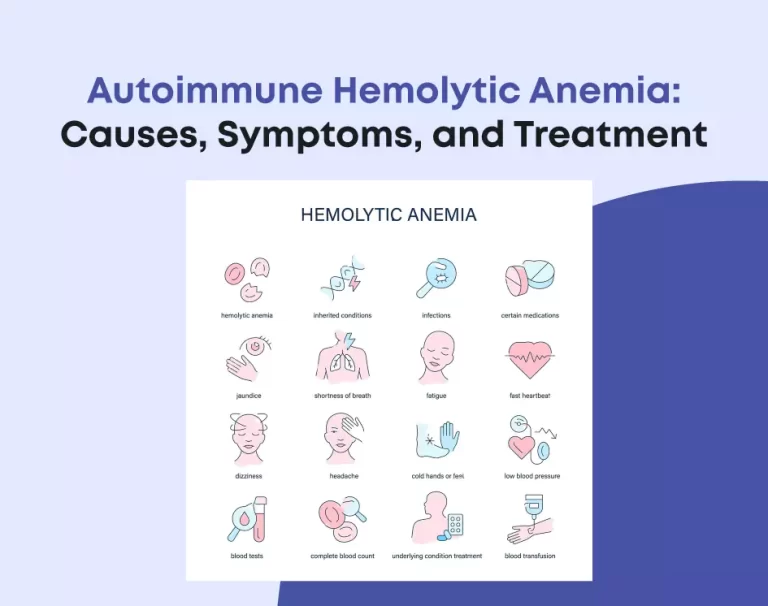
Autoimmune Hemolytic Anemia: Causes, Symptoms, and Treatment
Autoimmune hemolytic anemia (AIHA) occurs when the body’s immune system mistakenly attacks its own red blood cells, leading to their destruction. Red blood cells carry oxygen from the lungs to various tissues and organs in a healthy individual. However, the immune system identifies these cells as foreign invaders in AIHA. Therefore, it launches an attack, resulting in their premature destruction. This leads to a shortage of red blood cells, causing anemia. Anemia can result in symptoms such as fatigue, weakness, pale skin, shortness of breath, and rapid heartbeat.
Understanding Autoimmune Hemolytic Anemia
Understanding the mechanisms behind AIHA is crucial for effective management and treatment. It allows you to develop tailored strategies to suppress the immune response and preserve red blood cell function.
- Immune System Dysfunction:
The immune system erroneously recognizes red blood cells as invaders and launches an attack against them.
- Red Blood Cell Destruction:
Immune-mediated destruction of red blood cells leads to anemia.
- Impact on Oxygen Transport:
Anemia interrupts the body’s ability to transport oxygen to tissues and organs. As a consequence, individuals may experience symptoms like fatigue and difficulty breathing.
- Genetic Factors:
Certain genetic predispositions may increase the risk of developing AIHA.
- Autoimmune Disorders:
AIHA may occur in conjunction with other autoimmune conditions, such as lupus or rheumatoid arthritis.
- Environmental Triggers:
Exposure to certain environmental factors or toxins may trigger the onset of AIHA.
Knowing the mechanisms of autoimmune hemolytic anemia can better navigate its challenges and seek appropriate treatment.
Causes of Autoimmune Hemolytic Anemia
Autoimmune hemolytic anemia (AIHA) can have various underlying causes or triggers. Yet, in numerous instances, the precise cause remains elusive. Potential factors contributing to AIHA include underlying medical conditions. Certain medications or drugs, infections, genetic predisposition, autoimmune disorders, and environmental triggers can also lead to this.
- Underlying Medical Conditions:
Conditions like lupus, rheumatoid arthritis, and certain cancers may increase the risk of developing AIHA.
- Medications and Drugs:
Some medications, including certain antibiotics and anticoagulants, can trigger an immune response leading to AIHA.
- Infections:
Viral infections such as hepatitis and Epstein-Barr virus can sometimes trigger AIHA.
- Genetic Predisposition:
Genetic factors may play a role in predisposing individuals to develop AIHA.
- Autoimmune Disorders:
AIHA may occur in conjunction with other autoimmune conditions, such as lupus or rheumatoid arthritis.
- Environmental Triggers:
Exposure to certain environmental factors or toxins may trigger the onset of AIHA.
Exploring these potential reasons can provide insight into the triggers of autoimmune hemolytic anemia and guide treatment strategies. Identifying potential causes can tailor treatment plans to address the underlying factors contributing to autoimmune hemolytic anemia.
Symptoms of Autoimmune Hemolytic Anemia
Recognizing the symptoms of autoimmune hemolytic anemia (AIHA) is essential for prompt diagnosis and treatment. While symptoms can vary from person to person, common signs of AIHA include:
- Fatigue and Weakness:
Reduced oxygen transport due to anaemia can lead to fatigue and weakness.
- Pale or Yellowish Skin (Jaundice):
Increased breakdown of red blood cells can cause jaundice, leading to yellowish skin and eyes.
- Shortness of Breath:
Anemia can result in reduced oxygen delivery to tissues, causing shortness of breath.
- Rapid Heartbeat (Tachycardia):
The heart might increase its rate to compensate for the diminished oxygen levels in the bloodstream.
- Dark Urine:
Increased breakdown of red blood cells can lead to the presence of hemoglobin in the urine, causing it to appear dark.
- Enlarged Spleen:
Some individuals with AIHA may experience an enlarged spleen due to increased red blood cell destruction and removal.
Understanding these symptoms can help individuals and healthcare providers identify autoimmune hemolytic anemia early and initiate appropriate treatment. Early recognition of symptoms can lead to prompt intervention, improving outcomes for individuals with autoimmune hemolytic anemia.
Diagnosis of Autoimmune Hemolytic Anemia
Diagnosing autoimmune hemolytic anemia (AIHA) involves a comprehensive evaluation. It includes medical history assessment, physical examination, and laboratory tests. Healthcare providers may perform various blood tests, including a direct Coombs test, hemolysis tests, and possibly a bone marrow examination. These all can confirm the diagnosis and determine the underlying cause of AIHA.
- Blood Tests:
Blood tests are used to assess red blood cell count, hemoglobin levels, and markers of hemolysis.
- Direct Coombs Test:
This test detects antibodies attached to red blood cells, indicating immune-mediated destruction.
- Hemolysis Tests:
These tests assess the rate of red blood cell breakdown.
- Bone Marrow Examination:
In some cases, a bone marrow biopsy may be performed to evaluate red blood cell production.
Accurate diagnosis is essential for developing an effective treatment plan and managing autoimmune hemolytic anemia. Healthcare providers can accurately diagnose autoimmune hemolytic anemia through thorough evaluation and diagnostic testing and initiate appropriate treatment.
Treatment of Autoimmune Hemolytic Anemia
Treatment for autoimmune hemolytic anemia (AIHA) aims to suppress the abnormal immune response. Furthermore, this reduces red blood cell destruction and alleviates symptoms. Treatment options may include:
- Corticosteroids:
Such medications work by dampening the immune system’s activity and mitigating inflammation. They help to alleviate symptoms and prevent further red blood cell destruction.
- Immunomodulatory Drugs:
Drugs that modulate the immune system’s response may be used in severe or refractory AIHA cases.
- Blood Transfusions:
Transfusions may be necessary to replace lost red blood cells and improve oxygen delivery to tissues.
- Splenectomy:
Surgical removal of the spleen may be considered in certain cases to reduce red blood cell destruction.
- Immunoglobulin Therapy:
Intravenous immunoglobulin may be used to modulate the immune response and reduce red blood cell destruction.
Individualised treatment plans are developed based on the patient’s specific needs and response to therapy. With appropriate treatment and management, individuals with autoimmune hemolytic anemia can achieve an improved quality of life and symptom control.
Final Thoughts
Autoimmune hemolytic anemia is a complex condition that requires careful evaluation, diagnosis, and treatment. Learn about its causes, symptoms, and treatment options through this guide. Individuals and healthcare providers can work together to manage this condition and improve outcomes effectively. So, raise awareness and support research efforts to advance your understanding and treatment of autoimmune hemolytic anemia.