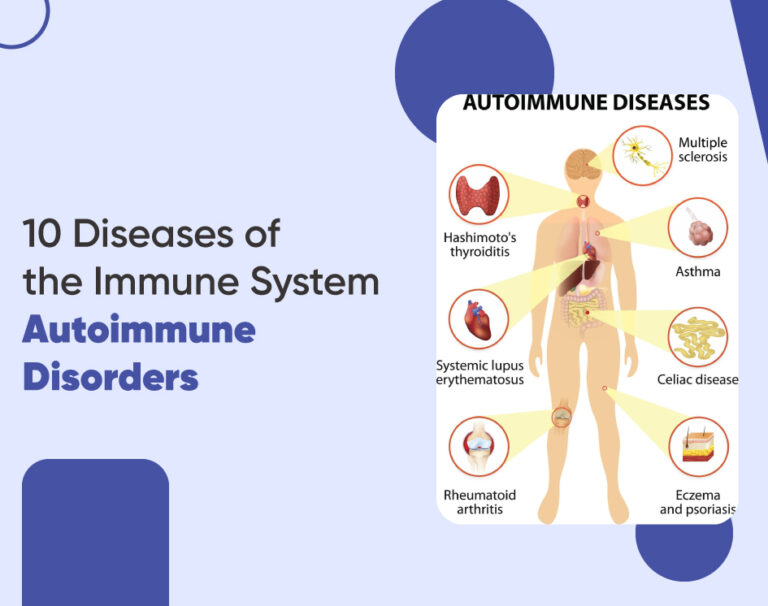
10 Diseases of the Immune System | Autoimmune Disorders
Our immune system is a complex network of cells, tissues, and organs that work together to defend your body against harmful invaders, such as bacteria, viruses, and parasites. However, in some cases, the immune system can malfunction and attack the body’s tissues, such as skin, joints, organs, and nervous system, leading to autoimmune disorders. These conditions can affect various parts of the body, causing a range of symptoms and complications. Here, we’ll explore 10 common autoimmune diseases and their impact on health.
Understanding Autoimmune Disorders
Autoimmune disorders occur when the body’s immune system mistakenly attacks its tissues, thinking they are foreign invaders. This can lead to a wide range of health issues, depending on which part of the body is affected. Among the various autoimmune disorders, some are more prevalent, such as Rheumatoid Arthritis, Lupus, and Multiple Sclerosis. These conditions can have a profound impact on an individual’s life, altering their daily activities and overall well-being.
Types of Autoimmune Disorders
Rheumatoid Arthritis (RA)
Rheumatoid Arthritis (RA) is a chronic inflammatory disorder affecting not just the joints but potentially a variety of body systems, including the skin, eyes, lungs, heart, and blood vessels. It is characterized by the immune system attacking the synovium, the lining of the membranes that surround the joints. The resulting inflammation can lead to joint damage and deformity. Symptoms include tender, swollen joints, and in some cases, RA may cause physical disabilities.
Systemic Lupus Erythematosus (SLE)
Systemic lupus erythematosus (SLE) is a systemic autoimmune disease that can impact various organs such as the skin, joints, kidneys, heart, and lungs. Symptoms can vary widely and may include fatigue, joint pain, skin rashes, and kidney problems.
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition in which the immune system attacks insulin-producing cells in the pancreas. This leads to a lack of insulin, a hormone necessary for regulating blood sugar levels.
Multiple Sclerosis (MS)
Multiple sclerosis (MS) is a chronic autoimmune condition that impacts the central nervous system, including the brain and spinal cord.In MS, the immune system attacks the protective myelin sheath that covers nerve fibers, disrupting communication between the brain and the rest of the body. This can lead to a wide range of symptoms, including fatigue, muscle weakness, numbness, and difficulty walking.
Inflammatory Bowel Disease (IBD)
IBD is a group of inflammatory conditions of the colon and small intestine, including Crohn’s disease and ulcerative colitis. These conditions cause chronic inflammation of the gastrointestinal tract, leading to symptoms such as abdominal pain, diarrhea, and weight loss.
Psoriasis
Psoriasis is a skin condition driven by autoimmunity, presenting as red, itchy, and scaly patches. It arises from our immune system’s misdirected attack on healthy skin cells, triggering their rapid proliferation. This leads to the development of thick, silvery scales and red patches on the skin. Treatment focuses on reducing inflammation, regulating skin cell growth, and alleviating symptoms.
Graves’ Disease
Graves’ disease is an autoimmune disorder characterized by the thyroid gland becoming overly active, resulting in hyperthyroidism. This condition manifests with symptoms like weight loss, rapid heartbeat, tremors, and fatigue. Treatment options include medications to lower thyroid hormone levels, radioactive iodine therapy, and surgery.
Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is an autoimmune disease that causes inflammation and damage to the thyroid gland, leading to an underactive thyroid (hypothyroidism). Symptoms of hypothyroidism can include fatigue, weight gain, constipation, and sensitivity to cold. Treatment involves thyroid hormone replacement therapy.
Celiac Disease
Celiac disease is an autoimmune condition triggered by consuming gluten, a protein present in wheat, barley, and rye. In individuals with celiac disease, gluten prompts an immune reaction that harms the lining of the small intestine, resulting in poor nutrient absorption. Symptoms may include diarrhea, abdominal discomfort, bloating, and fatigue. Treatment entails adhering to a gluten-free diet.
Autoimmune Hemolytic Anemia
Autoimmune hemolytic anemia (AIHA) is a rare autoimmune disorder in which the immune system attacks red blood cells, leading to their destruction and resulting in anemia. Symptoms of AIHA can include fatigue, pale skin, jaundice, and shortness of breath. Treatment may include corticosteroids, immunosuppressants, and, in severe cases, blood transfusions.
Common Symptoms of Autoimmune Disorders
While the symptoms of autoimmune disorders can be diverse and affect various organs, there are common symptoms that many people with these conditions experience. Recognizing these symptoms can be crucial for early diagnosis and management.
Fatigue
Fatigue is one of the most common symptoms across various autoimmune disorders. Individuals may feel constantly tired, regardless of how much rest they get. This type of fatigue can significantly impact daily activities and quality of life, making even simple tasks seem impossible.
Joint Pain
Joint pain is a frequent complaint among those with autoimmune disorders, especially in conditions like Rheumatoid Arthritis and Lupus. The pain can range from mild to debilitating and is often associated with inflammation and swelling, causing discomfort and limited mobility.
Skin Rashes
Many autoimmune disorders can cause skin rashes as a result of inflammation in the skin. Lupus, for instance, is well-known for causing a butterfly-shaped rash on the face. These rashes can be itchy and painful and may also serve as a visual indication of the underlying immune system activity.
Causes of Immune System Diseases
The genesis of immune system diseases, particularly autoimmune disorders, is complex and not entirely understood. However, research has identified two primary factors that significantly influence the development of these conditions: genetics and environmental triggers.
Genetics
Genetics plays a pivotal role in autoimmune diseases. A family history of such disorders often increases the risk of an individual developing the same or similar conditions. Specific genes linked to the immune system can make a person more susceptible to autoimmunity. For instance, specific genetic markers are associated with higher risks of diseases like rheumatoid arthritis, lupus, and multiple sclerosis. Despite this genetic predisposition, not all individuals with these genetic markers will develop an autoimmune disorder, suggesting that other factors also contribute to disease onset.
Environmental Factors
Environmental factors are significant triggers for autoimmune diseases, especially among genetically predisposed individuals. These factors include:
Viral and bacterial infections: Certain infections can trigger autoimmune responses. For example, the Epstein-Barr virus is linked to multiple sclerosis and lupus.
Sunlight: UV radiation can exacerbate symptoms of diseases like lupus.
Chemical exposure: Exposure to certain chemicals, including those in cigarettes or pesticides, has been associated with a higher risk of autoimmune diseases.
Diet and nutrition: Some studies suggest that high salt intake, gluten, and other dietary factors may play a role in autoimmune disease development.
Diagnosis
Effective management of autoimmune disorders hinges on timely diagnosis and appropriate treatment strategies, which can vary widely based on the specific disease and severity of symptoms.
Blood Tests
Blood tests are a fundamental part of diagnosing autoimmune diseases. These tests typically look for specific antibodies that the body produces in response to an autoimmune condition. For instance, antinuclear antibody (ANA) tests can help diagnose lupus. In contrast, rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) tests are used for rheumatoid arthritis. Elevated levels of specific inflammatory markers, like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), can also indicate an autoimmune response.
Treatment Options for Autoimmune Disorders
Medications
Medications play a crucial role in managing autoimmune disorders, aiming to reduce symptoms, control the autoimmune response, and maintain the body’s ability to fight diseases. Common medications include:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to alleviate pain and inflammation.
- Immunosuppressants that help control the immune system’s activity.
- Corticosteroids reduce inflammation and suppress immune system activities.
The choice of medication often depends on the specific autoimmune disease and the patient’s overall health condition.
Lifestyle Changes
Lifestyle modifications can significantly benefit individuals with autoimmune diseases by improving overall well-being and reducing disease flare-ups. Recommended changes include:
- Following a well-rounded diet that includes plenty of fruits, vegetables, whole grains, and lean proteins.
- Regular physical activity to strengthen muscles, improve mood, and boost overall health.
- Adequate rest and stress management techniques, like meditation and yoga, to help mitigate the effects of stress on the body.
- Avoiding known triggers, such as certain foods or prolonged sun exposure, that can exacerbate symptoms.
By combining medical treatments with lifestyle adjustments, individuals with autoimmune disorders can lead healthier, more comfortable lives.
Conclusion
In conclusion, autoimmune diseases are a complex group of disorders that can affect virtually any part of the body. While these conditions cannot be cured, treatment options are available to help manage symptoms and improve quality of life. Timely identification and treatment are crucial for effectively managing autoimmune conditions and averting complications. If you suspect you may have an autoimmune disease, it’s necessary to consult with a healthcare professional for proper evaluation and management.